Due to developing a mild case of OHSS, my doctor switched me from doing a fresh embryo transfer to a frozen embryo transfer (FET). After my egg retrieval, my eggs were fertilized and then frozen once the embryos grew to either day five or day six blastocysts. I ended up with 11 total frozen embryos. From there, I had to wait what seemed like forever to get a consultation with my reproductive endocrinologist (RE) to go over my Frozen Embryo Transfer Cycle Protocol, decide on the number of embryos to transfer, and set a tentative date for the embryo transfer. Not all FET cycles and protocols are the same; however, I am sharing mine with you to give some insight into how these cycles go.
Related: What I did to Ensure I had a Successful IVF Cycle
Frozen Embryo Transfer Cycle Medications
FET cycle protocols are a lot less “work” in comparison to stimulation cycles. I say that because there are practically no injectable medications and a lot fewer visits to the doctor. This means less invasive transvaginal sonograms, which with a stim cycle can occur every other day.
The medications that were prescribed to me for my frozen embryo transfer cycles were as follows:
- Estrace – This is an oral form of estrogen, which was used to increase the amount of estrogen my body produced in order to prepare the endometrial lining of my uterus. A thicker endometrial lining is needed and is the perfect environment for embryo plantation.
- Progesterone – Progesterone can be taken vaginally, as an intramuscular injection in the buttocks, or both in order to maintain an early pregnancy. I was lucky enough to be prescribed both oral (Endometrin) and intramuscular injections (progesterone in sesame oil).

Endometrin was administered twice daily in the morning and evening, while the progesterone in oil (PIO) was administered every three days. For the injections, I had zero at-home assistance from my husband because he has an aversion to needles; therefore, a few of the [weekend] shots were given to me at my REs office. I was thankful enough to have a willing nurse friend/co-worker administer my injections during the week. I still have to get her a nice gift as a ‘Thank You’ so if you have any ideas, leave it as a comment below.
Make Sure You Get Your Medications In Advance
All of these medications were obtained prior to the start of my menstrual cycle to ensure that I was able to start the medications timely. With any type of artificial reproductive treatment (ART) timing is always of the essence.
Frozen Embryo Transfer Cycle Protocol
Similar to IVF stimulation cycles, the party gets started on the first day of your menstrual cycle. On the first day of my cycle, I was instructed to contact my REs office to schedule an appointment for Cycle Day (CD) 2 or CD3 to come in for bloodwork, sonogram and to review my upcoming weeks of treatment.
Related: My IVF Process: How We Got Our Rainbow Baby
The sonogram done during CD2 or CD3 would provide a baseline measurement of my uterine lining (endometrial lining) and antral follicle count (AFC). Other office visits scheduled during my FET Cycle were to ensure my lining was developing appropriately to accept an embryo for transfer and to adjust medication dosage, if necessary.

Related: What to Look for When Searching for a Reproductive Endocrinologist
I took Estrace from CD2 through CD10 until I was seen again for a sonogram to check on my lining, estrogen, and progesterone levels. I continued taking the Estrace from CD10 through CD12 before being seen again at my REs office. This went on again, taking Estrace from CD12 through CD 14 with another office visit to measure my lining and hormone levels. On CD14 something happened that really wasn’t supposed to due to the medications I was taking; I ovulated.
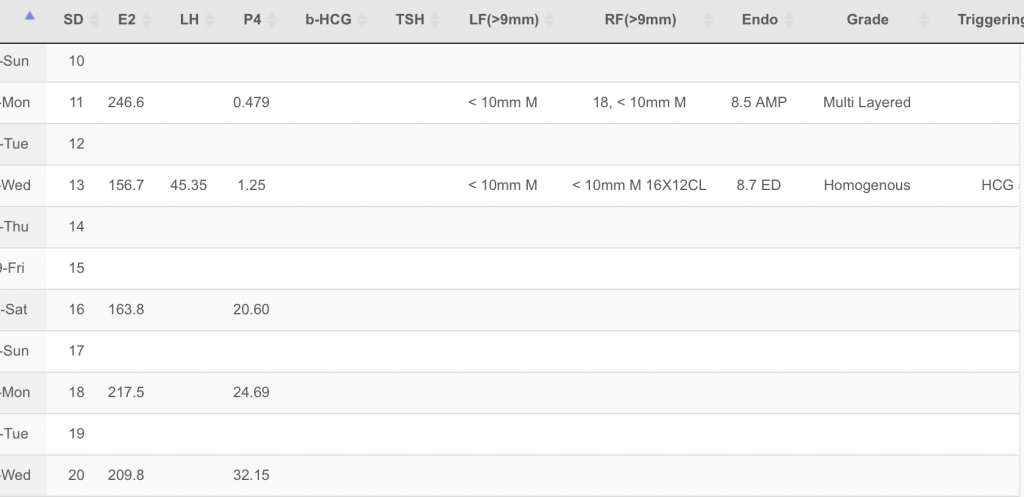
I normally ovulate on my own; however, estrogen is supposed to prevent that from happening during a FET cycle. Due to my ovulating, I was rushed into my REs office mid-day for a 5,000-unit subcutaneous injection of hCG and a 50mg intramuscular injection of PIO. The hCG was given to “prime” my uterus for the transfer, which as a result of this was moved up one day.
Over the next few days, from CD14 through CD17 I continued taking Estrace with the addition of Endometrin 400 mg per day. On CD17, which was two days before transfer, in addition to those medications, I was given a shot of PIO. CD 18 and CD19 I took Endometrin twice per day along with Estrace. CD19 was my frozen embryo transfer day!
Frozen embryo transfers are usually scheduled on CD19 when the uterine lining is triple lined and approximately >7.5 mm thick. On transfer day, my uterine lining was 8.7 mm thick. My current pregnancy is an indication that was the perfect thickness to accept the embryo transferred.
Below is a calendar that shows each medication taken for my Frozen Embryo Transfer Protocol

Frozen Embryo Transfers are quick, as long as the embryo cooperates. Unfortunately, for me, that wasn’t the case. But I will get into that in another post where I share my frozen embryo transfer story. So stay tuned!

